A Day in an Ebola Treatment Unit
Originally written March 1, 2015
The only word I have been able to find to describe this experience so far is surreal. Today it became real for me.
Today was our first day actually treating patients in Maforki, Partners In Health’s Ebola Treatment Unit (ETU). Yesterday we set foot there for the first time, donned and doffed our protective suits twice to get a tour of the Red Zone, but didn’t do much actual patient care since we were still getting oriented. Today we were buddied up with more experienced clinicians and assigned specific patients to care for during our shift. Today Ebola ceased to be a faceless mass of African suffering, and became two individual human beings.
I’ll give you all the lay of the land at Maforki before we get much further. Maforki ETU belongs to the Sierra Leonean government, unlike many Ebola centers that were constructed from the ground up by the nonprofits that came to run them. When PIH arrived in Port Loko at the peak of the outbreak last October, they were the only international health workers in the entire district, which had 150 confirmed Ebola cases and zero adequate facilities in which to treat them. The Maforki ETU had been converted from a school and was overflowing with patients literally dying for care. When PIH staff came to tour it to learn about how to construct an ETU, the Sierra Leonean health minister stopped them in their tracks. He was tired of international groups coming to tour government ETUs, telling them what was wrong, and then leaving to build their own instead of fixing the existing centers from the inside. He insisted that his people could not wait 8 weeks for care while PIH constructed their own center. He wanted them to start working in Maforki the next day. PIH could see that he was right, and they have been doing the best they can with what they have at Maforki ever since.
Maforki is a built out around what used to be a school before the outbreak. The patient wards were once classrooms, large concrete buildings painted red on the outside, with several beds in each. When it was converted to an ETU, additional basic structures were added at the periphery: a triage area, nurses’ station, meeting room, areas for donning and doffing personal protective equipment (PPE). Nailed together out of mismatched wood and blue tarps, the whole thing looks a bit ramshackle, but the center is known in the area for giving excellent care. I’m told that Port Loko residents who fear they might have Ebola ask to be brought to Maforki because they have heard they’ll be treated well.
The whole center is divided into two main areas: the Green Zone and the Red Zone. The clinicians’ areas are in the Green Zone, so we can have meetings, draw up medications, eat meals, etc in an area that is not contaminated with the virus. The patient wards are in the Red Zone. No one steps one foot into the Red Zone for any reason unless they are in full PPE, and nothing you take into the Red Zone is allowed to come out. To enter the clinician’s area from the outside, we must dip the bottoms of our shoes in a bucket of chlorine, wash our hands in chlorine, and have our temperatures taken at the gate. Fever is an early sign of Ebola, and we want to be sure that no one entering the Green Zone might be contagious.
At the beginning of each shift, the staff gathers in front of a large white board displaying the names and medical information of each of our patients. Today there were ten (five confirmed Ebola, and five suspect). We discuss how each one fared overnight, and divide them up between the nurses. My group of nurses was assigned to the confirmed Ebola patients, so we huddled at the nurses’ station to make a plan.
Because we are limited to 90 minutes in our PPE for safety and health reasons, we need to decide everything we’re going to do before we enter the Red Zone. We also need to be thoughtfully gather any supplies we might need, since there’s no way to step back out of the Red Zone to grab something once you’re inside. The Suspect Ward does have a wooden slide from the window of the supply room in the Green Zone crossing over the fence into the Red Zone, so if we need something we can ring the bell on the Red Zone side and someone will slide whatever we need down to us. But again, that just wastes time in your suit.
So my team drew up all of the medications we thought we’d need and packed up IV start supplies, plenty of bags of IV fluid, rags, and lapas (beautiful African fabrics used for just about everything, but in this case as sheets). I found myself giving doctors tips on how to draw up meds, since at home they are normally the ones writing orders, while nurses actually carry them out. Here in Maforki, however, it’s all hands on deck and the doctors gladly perform nursing care with the rest of us. Since one of our patients had just been confirmed Ebola positive this morning, we would need to move him from Suspect to the Confirmed Ward. We had been told he was too sick to walk, so we improvised with our limited resources and brought a body bag to put him on so we could carry him.
Then it was time to don our PPE. I hunted for two pairs of gloves in my size, as well as a pair of black rubber boots that fit me, out of the many drying on a rack in the sun outside the nurses’ station (exposure to sunlight kills the virus). Then I joined the rest of my team in the donning room, the last stop before we entered the Red Zone. A few Sierra Leonean staff double-checked us as we donned our suits. They cut thumb holes in the sleeves so they wouldn’t ride up and expose our wrists, and sprayed de-fogger on the inside of our face shields. I felt myself start to sweat as soon as I zipped my gown up. Ninety-degree days and no air conditioning makes for a sweltering environment inside the PPE, but there’s no other way for us to protect ourselves. After writing “Emily, Nurse” on the front and back of my suit, staff jotted down the time we were entering the Red Zone on our sleeves, and literally gave us a stamp of approval on our forearms. We were ready to go in.
As we walked through the doorway into the Red Zone, I took up the “Ebola pose” that we had been taught in training – interlocking my fingers in front of me at about the height of my navel, to discourage me from reaching up to touch my face or anything else around me. One of the Maforki nurses told me that when he’s in the Red Zone he pretends he’s playing a giant game of Operation, trying not to touch anything around him that he doesn’t have to. He assumes that every surface is contaminated with Ebola.
The Red Zone is designed to flow from lowest to highest risk, so the first ward we came to was Suspect. The Suspect patients (who have Ebola symptoms but have not yet had a positive test) are divided between those who have dry symptoms (fever, headache, hiccups, weakness, etc) and those who have wet symptoms (vomiting, diarrhea, and bleeding). The idea is to decrease the likelihood that one patient will infect another with Ebola. The disease has vague symptoms, so sometimes patients turn out to just have malaria or Lassa fever – we don’t want patients coming to the ETU without Ebola, and catching it there.
The facilities are rudimentary, to put it mildly. There is no running water, and electricity is unreliable. “Wet” patients produce a huge amount of highly infectious diarrhea and are often too weak to reach the toilets. Many wards have old cholera beds, which have a large hole at the center that patients can position themselves over, with a bucket on the floor underneath to catch their waste.
Unfortunately Maforki does not have its own lab, so we send our blood samples to another nonprofit which runs our lab tests and emails us the results. The process can take 12-36 hours. In the meantime, all suspect patients must be housed within the Red Zone in case they do turn out to be Ebola positive. We don’t get many patients who return after they’ve been discharged negative, which is reassuring.
We did have an 11-year-old girl in the suspect ward today who was here for the second time. She came to triage once before and was admitted to Suspect because her symptoms met the case definition for Ebola. She turned out to be negative and was sent home after a few days, but because she spent time in an ETU, she had to be followed as a “contact” for 21 days. At some point during that monitoring period, she spiked a fever again and was brought back to us.
A fever by itself isn’t cause for alarm, but fever plus a history of contact with an Ebola patient is one of the case definitions that makes a person an Ebola suspect. Since she’d had contact with Ebola patients in the last three weeks, we had to re-admit her and test her again. On my first round of the day, I found her sitting in the alone in the courtyard of the Suspect ward, where I imagine dozens of children used to play during recess at school. We brought her a fresh bottle of cold water and encouraged her to drink but she refused. All I wanted to do was comfort her, but it’s incredibly hard to connect with a child from inside a suit that makes you look like a monster. Fortunately her test came back negative today, and we sent her home for another 21 days of monitoring.
Another of our patients today was not so lucky. Foday* was brought to Maforki yesterday already very ill, and his test came back positive for Ebola this morning. We needed to move him from Suspect to the Confirmed ward. When my team of four clinicians entered the Suspect Wet ward, we found Foday curled in bed in his own waste. We carefully cleaned him up, stepping over to a “sprayer” who followed us with a tank of chlorine on his back to rinse our outer layer of gloves whenever they were visibly soiled.
Once Foday was as clean as we could get him, we rolled him onto the body bag we had brought with us and lifted him out of bed. Communicating with each other the entire time, we made our way out of the Suspect ward, through the gate into the Confirmed area, and lay him down on a bed in a room with the other Confirmed patients.
In the bed next to Foday lay 10-year-old Abass. When we visited him yesterday he had barely responded, and we worried over the bleeding we saw at his gums – a late sign, and not a reassuring one. Today he was reaching out for something with both hands; I imagined a family member whose presence he was hallucinating. The team before us had given him his meds, but I couldn’t help walking over to him to try to give him some comfort. When I entered his field of vision he recoiled. Between the language barrier and his delirium, I couldn’t explain to him why his family wasn’t there to wipe his face and hold his hand, and he was instead being cared for by a stranger dressed like an alien.
Having used up a lot of our allotted time already, we went to work giving Foday his medications. At Maforki we are aggressive with IV fluids, although it’s difficult because we can only administer them while we are inside the unit with the patients. Experience has shown that if we hook up an IV line and leave it hanging, we will return a couple of hours later to find that the patient has accidentally ripped it out and bled everywhere. Unfortunately there just aren’t enough trained staff to have clinicians at the bedside 24/7. So we did the best we could with the time we had left, giving Foday IV fluids, antibiotics to prevent secondary infections, artesunate for malaria, and paracetamol for his fever. Although we had cleaned him up after he’d soiled himself again, by the time we had to leave he was already lying in his own diarrhea for the third time since we’d arrived about an hour before. With no time left, we had to leave it for the next round of clinicians.
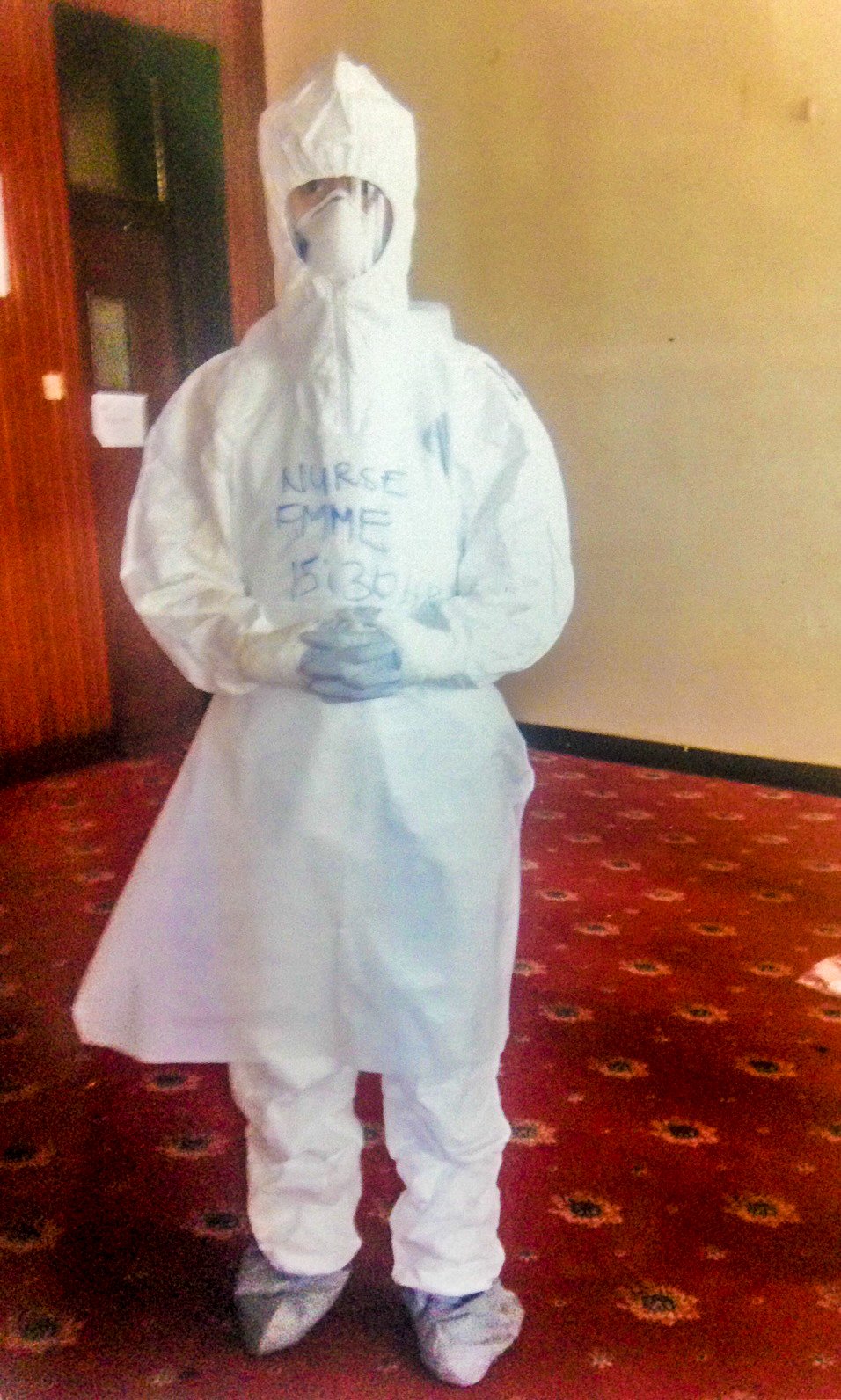
A typical doffing station in an Ebola Treatment Unit in Sierra Leone
Although we technically can spend 90 minutes in the PPE, a good chunk of that is taken up by the doffing process. As I’ve mentioned before, removing our PPE is the point at which we’re most likely to contaminate ourselves and contract Ebola. We have infectious body fluids all over us, and we have to get out of our suits without getting a speck of it on ourselves. Doing it correctly takes 20-30 agonizing minutes. Here’s the process:
I approach a national staffer in full PPE who has a tank of chlorine on his back attached to a sprayer, and as he sprays I wash my hands (or rather, my outer layer of gloves) for one full minute. He then sprays the whole front of my suit, and then asks me to turn around so he can spray the back. When he’s finished, I tear off my apron very carefully so that the pieces don’t snap and flick any fluid at me. Then I wash my gloves with the chlorine sprayer for a full minute again.
Next I move to my doffing station, where I stand in a bucket of chlorine and shuffle my feet for a full minute, to kill the virus on my boots. I step out of the bucket and into my doffing station, where a bucket full of chlorine with a tap awaits on top of a wooden table. I open the tap and wash my outer gloves again for a full minute, making sure to keep some chlorine in my hands at the end to splash on the tap, so I don’t pick up any virus that I left there when I turned it on.
I step over to a full length mirror leaned against the wall and slowly, carefully unzip my suit and then pull the hood back off of my head. I wriggle the suit down my torso, past the top of my boots onto the ground, making sure to only touch the outside. I then pull my hands forward, letting my sleeves roll off and my top layer of gloves with them.
Now my suit is off except for my feet, so I do the “Ebola dance” and shuffle my boots out of the ankles of my gown. Then I carefully nudge the suit over to a sprayer on the Green Zone end of the doffing station, who waits until I turn away to spray it down with chlorine (we don’t want anything splashing into our eyes). While he sprays my suit, I step back into the chlorine bucket and clean my boots again. Once my suit is sprayed, I pick it up with one gloved hand and deposit it in a large trash can (I still have my inner layer of gloves on at this point).
My suit safely disposed of, I now return to the chlorine station and wash my remaining pair of gloves for a full minute. Then back to the mirror, where I ever so carefully grasp my face shield with both hands, pull it as far away from my face as I can, turn my face the other way with my eyes closed, and remove it. Back to the chlorine station to wash my gloves for another minute. Next it’s the same process with my face mask, pulling it far away and turning my face so that if anything splashes, it won’t go into my eyes, nose or mouth. Then another minute of hand washing.
All that’s left at this point is my final layer of gloves, which I remove at a glacial pace. The goal is to never touch my hands with the dirty outside surface of the gloves. Try putting on some gloves, dipping them in mud, and then getting them off without getting ANY on your hands. It’s tougher than it sounds.
My buddy clinician, still in PPE, stands in the Red Zone and supervises me through this entire process to make sure nothing is missed. Once my equipment is off, I approach the chlorine sprayer in the Green Zone, who sprays the front of my boots, asks me to turn, sprays one side, asks me to turn again, sprays the other side, then asks me to turn around so they can spray the back. I then lift one foot at a time while they spray the soles of my boots as I slowly back out from the Red Zone into the Green Zone.
With all of my PPE finally off and my boots clean, I wash my hands for a full minute with chlorine, and then again for a minute with soap and water. To be extra safe, I’m not supposed to touch my face for the next half hour.
By now it’s almost noon, and we head to the nurses station to re-hydrate and have a snack before our second round in the Red Zone. Physically, I’m feeling fine. I seem to be one of the lucky ones who is surprised when our time is up, and I come out of my PPE almost as dry as I went in while others emerge with their scrubs a shade darker from top to bottom with sweat.
Emotionally, it’s harder.
By our second round in the afternoon, Foday was looking worse. He was having pretty much constant diarrhea, rolling over to vomit into a bucket next to his bed, and dripping blood from his nose. His fever had risen and he was tachycardic. Dried blood was caked all over his nose and mouth. We started a second IV and rushed fluids into him, and tried to clean him up from head to toe.
At some point he decided he was done putting up with all of these white-suited monsters poking at him, so he rolled over and tried to stand up, clearly agitated and confused. With two IVs hooked up and blood running down his face, any quick movement on his part would mean spraying infectious fluids all over the place. As a nurse, everything in my heart wanted to go rub his back, help him back into bed, and calm him down enough that we could continue to care for him – while everything in my brain was shouting, “Get away from him!” Suddenly my PPE seemed so fragile. Foday eventually calmed himself down and crawled back into bed, and I was left feeling surprised and ashamed at how afraid I’d been.
Most of the clinicians who have been here a while think Foday is too far gone to recover. If they’re right, I hope he passes away soon. I’m heading back to Maforki shortly for an evening shift, and I know we’ll do everything we can to make him comfortable. Even if he is going to die, he doesn’t have to die in pain and covered in his own mess.
Night shift tells us little Abass is looking better today, and I’m looking forward to seeing him for myself. I hope that telling Abass and Foday’s stories stories has put faces to the outbreak. The numbers we hear on the news are people, every one of them just as important as us and our families.
I will never understand why some people’s lives seem to matter more than others. Why, if I get sick, will I be flown home to receive the best medical care in the world, while Foday is dying in his own filth as we do what we can for him with the little we have?
Next Post: Abass’s Smile
Previous Post: Trained and Ready
*All names changed to protect privacy
You Might Also Like:
This post contains affiliate links. This means that if you decide to make a purchase through any of the links we recommend, we get a small commission at absolutely no cost to you. This helps with the cost of keeping this site running – so thank you in advance for clicking through! And not to worry, we don’t recommend anything we don’t fully believe in or that doesn’t align with our values.